Articles > Common Urological Conditions
Minimally invasive surgery refers to a surgical technique that allows access to internal organs and tissue without the need for a large incision. Instead, small incisions, usually less than one centimeter in size, are made to insert miniaturized instruments and a camera called a laparoscope.
The major advantage of this approach is that it enables surgeons to have remote viewing and confirmation of conditions within the body. The laparoscope provides high-definition images of the surgical site, allowing the surgeon to visualize and identify any abnormalities or issues that need attention. This real-time visual information helps the surgeon make precise and accurate decisions about the corrective procedures that are needed.
By utilizing this method, surgeons are able to minimize trauma to the body and reduce the risk of complications associated with traditional open surgery. Patients can expect shorter hospitalization periods, faster recovery times, and reduced pain and scarring.
Overall, minimally invasive surgery revolutionizes the way surgical procedures are performed by maximizing patient outcomes through remote viewing capabilities and less invasive techniques. This approach has become increasingly common in various surgical specialties due to its proven benefits in terms of patient safety and positive postoperative outcomes.
Minimally invasive surgery plays a crucial role in the field of urology, as it offers numerous benefits compared to traditional open surgery. One of the key advantages is the reduction in pain experienced by patients undergoing minimally invasive procedures. By using smaller incisions and specialized instruments, surgeons can navigate and operate within the body with minimal disruption to surrounding tissues. This not only leads to reduced pain during the procedure but also post-operative pain, allowing patients to recover more comfortably.
Another significant benefit of minimally invasive urologic surgeries is the minimal scarring that occurs as a result. Open surgery often leaves large, visible scars as a result of the sizeable incisions required. In contrast, minimally invasive techniques result in much smaller incisions, leading to smaller, less noticeable scars. This not only improves the physical appearance of patients but also reduces the psychological distress often associated with prominent surgical scars.
Additionally, minimally invasive surgery significantly reduces the recovery time compared to open surgery. The smaller incisions result in less tissue trauma and damage, allowing the body to heal more quickly. Patients can often resume their normal activities much sooner, leading to a faster return to work and overall improved quality of life.
Minimally invasive urologic surgeries also offer several other benefits. They typically require less opioid use for pain management, which is especially important in the context of the ongoing opioid epidemic. Additionally, patients undergoing minimally invasive procedures tend to have shorter hospital stays, resulting in reduced healthcare costs and greater overall efficiency.
There are various methods of minimally invasive urologic surgeries. Catheter-based procedures, such as ureteroscopy, involve inserting a thin tube through the urethra to access and treat urological conditions. Laparoscopy, on the other hand, utilizes small incisions to insert a camera and instruments, allowing for precise and minimally invasive procedures. Lastly, robotic technology, such as robotic-assisted laparoscopic surgery, provides enhanced dexterity and precision for surgeons, further improving the outcomes of minimally invasive urologic procedures.
In conclusion, the importance of minimally invasive surgery in urological conditions cannot be overstated. It offers pain and scarring reduction, shorter recovery times, reduced opioid use, and shorter hospital stays. The various methods, including catheter-based procedures, laparoscopy, and robotic technology, contribute to the success of minimally invasive urologic surgeries. Embracing these techniques not only benefits patients but also enhances the overall efficiency and effectiveness of urological healthcare.
Minimally invasive techniques have revolutionized the field of medicine, providing patients with a range of benefits over traditional open surgeries. These procedures are characterized by small incisions, which reduce the risk of infection, minimize blood loss, and facilitate a speedier recovery. Instead of large open incisions, surgeons use specialized instruments and a laparoscope or endoscope to visualize and perform the necessary surgical interventions. The overview of minimally invasive techniques encompasses a vast array of specialties, including laparoscopic and robotic surgeries, endovascular procedures, interventional radiology, and arthroscopic surgeries, among others. This approach is steadily gaining popularity across medical disciplines due to its potential in reducing operative trauma, post-operative pain, hospital stays, and scarring. However, it necessitates advanced training and expertise for physicians and may not be suitable for all patients or conditions. Understanding the scope, advantages, and limitations of minimally invasive techniques is crucial for healthcare professionals and patients alike to make informed decisions and optimize patient outcomes.
At Children's Hospital of Philadelphia (CHOP), a range of laparoscopic urology procedures are offered to provide minimally invasive treatment options for pediatric patients. These procedures include orchiopexy, hernia repair, partial nephrectomy, total nephrectomy, nephroureterectomy, pyeloplasty, ureteral reimplantation, and removal of a renal cyst.
Orchiopexy is performed to correct undescended testicles, while hernia repair addresses the protrusion of abdominal tissue or organs through a weak area in the abdominal wall. Partial nephrectomy involves removing a portion of the kidney, while total nephrectomy involves complete removal of the kidney. Nephroureterectomy is the removal of a kidney and the attached ureter. Pyeloplasty corrects a blockage or narrowing in the ureteropelvic junction. Ureteral reimplantation is performed to address abnormalities in the ureter's connection to the bladder. Lastly, the removal of a renal cyst involves extracting a fluid-filled sac from the kidney.
Laparoscopic urology procedures offer several advantages over traditional open surgery. Patients tend to experience a faster recovery time, thanks to smaller incisions and reduced trauma to surrounding tissues. This minimally invasive approach also leads to shorter hospital stays, allowing patients to return home sooner. Moreover, laparoscopic surgery enables a quicker return to normal activities and less post-operative pain. Overall, the benefits of laparoscopic urological surgery at CHOP are evident in improved patient outcomes and enhanced quality of life.
Keywords: laparoscopic urology procedures, orchiopexy, hernia repair, nephrectomy, nephroureterectomy, pyeloplasty, advantages of laparoscopic surgery.
Laparoscopic surgery, also known as minimally invasive surgery, is a technique used to perform various urological procedures with smaller incisions, resulting in reduced pain, shorter hospital stays, and quicker recovery times.
The main components of laparoscopic surgery for urological conditions involve keyhole instrumentation and telescopic evaluation of the urinary tract. Keyhole instrumentation refers to the use of specialized tools specifically designed for laparoscopic surgery. These instruments are inserted through small incisions, typically 0.5-1 cm in length. They often consist of long, thin rods with attached surgical instruments, such as scissors or graspers, that can be manipulated within the body.
Telescopic evaluation involves the use of a laparoscope, which is a long, narrow tube with a light and camera at its tip. The laparoscope is inserted through one of the small incisions, allowing the surgeon to visualize the surgical site on a monitor. This enables a detailed examination of the urinary tract, including the kidneys, bladder, and ureters.
The benefits of laparoscopic surgery for urological conditions are numerous. Firstly, the smaller incisions result in reduced post-operative pain compared to traditional open surgery. This can lead to decreased use of pain medications and a quicker return to normal activities. Additionally, the shorter hospital stay is attributed to the reduced trauma to the body, resulting in fewer complications and a quicker recovery. Overall, laparoscopic surgery offers patients a less invasive option for urological procedures, leading to improved patient outcomes and satisfaction.
Introduction:
Laparoscopic surgery has revolutionized the field of urology by providing numerous benefits for the treatment of various urological conditions. This minimally invasive surgical technique has gained popularity among both patients and surgeons due to its advantages over traditional open surgeries. By making small incisions and using specialized instruments, laparoscopic surgery allows for faster recovery, reduced pain and scarring, shorter hospital stays, and improved cosmetic outcomes. Additionally, it offers better visualization of the surgical site, enabling surgeons to perform intricate procedures with greater precision and accuracy. With these compelling benefits, laparoscopic surgery has significantly improved patient outcomes and satisfaction, making it a preferred option for treating urological conditions.
Robotic surgery has revolutionized the field of urology, offering numerous benefits and applications. One key advantage is its ability to facilitate complex surgical reconstruction. Robotic-assisted surgery enables urologists to perform intricate procedures with enhanced precision and dexterity. This is particularly beneficial in cases like prostate cancer, where complex reconstruction of the urinary tract may be necessary.
Another advantage is that robotic surgery can reproduce a surgeon's hand and wrist motions with exceptional accuracy. This means that experienced surgeons can achieve the same level of control and precision as in traditional open surgery, but with minimally invasive incisions. Robotic instruments can move and rotate in a way that closely mimics human hand motions, facilitating precise sutures and delicate tissue manipulation.
Furthermore, robotic surgery provides a three-dimensional view of the surgical field, enhancing depth perception and spatial awareness. This clear and magnified visualization allows surgeons to navigate complex anatomical structures with confidence and perform intricate procedures with greater accuracy.
Additionally, robotic surgery minimizes trauma to the surrounding tissue. The robotic instruments are articulated, meaning they can move with a greater range of motion and flexibility than human hands. This allows for smaller incisions and less damage to healthy tissue during the procedure. Minimizing tissue trauma leads to reduced pain, shorter recovery times, and fewer complications for patients.
In summary, robotic surgery has numerous benefits and applications in urology, including facilitating complex surgical reconstruction, reproducing surgeon's hand and wrist motions, providing a 3D view of the surgical field, and minimizing trauma to tissue. Its advantages have improved patient outcomes and expanded the possibilities for intricate urological procedures.
Robotic surgery in urology is an innovative and highly advanced surgical technique that has revolutionized the field of complex reconstruction. It involves the use of a robotic surgical system that replicates a surgeon's hand and wrist movements with remarkable precision, all while providing a magnified, high-definition 3D view of the surgical site.
One of the key benefits of robotic surgery in urology is the minimal tissue trauma it causes. Traditional open surgeries often require large incisions, leading to significant damage to surrounding tissues. In contrast, robotic surgery utilizes small incisions, reducing the trauma to the patient's body. This results in less pain, decreased risk of infection, and shorter hospital stays.
Additionally, robotic surgery in urology is associated with a faster recovery period. The minimally invasive nature of the procedure accelerates the healing process, allowing patients to return to their normal activities sooner than with traditional surgery. This is particularly important for individuals undergoing complex urologic reconstructions, as it enables them to resume a better quality of life more quickly.
In conclusion, robotic surgery in urology offers numerous advantages, including complex reconstruction capabilities, the ability to replicate a surgeon's hand and wrist movements, a 3D view of the surgical site, minimal tissue trauma, and faster recovery. This revolutionary technique is transforming the field of urologic surgery and improving patient outcomes.
Advantages of Robotic Surgery Over Traditional Methods
Robotic surgery has revolutionized the field of medicine, offering numerous advantages over traditional surgical methods. With the use of robotic technology, surgeons are able to perform complex procedures with more precision and control. The robot's arms can make smaller and more precise incisions, leading to less trauma, bleeding, and scarring for patients. Additionally, the enhanced visualization provided by robotic systems allows surgeons to see the surgical site in 3D, providing a more comprehensive view and enabling a higher level of accuracy. The instruments used in robotic surgery also have a greater range of motion and dexterity, enabling surgeons to navigate tight spaces with ease and perform delicate maneuvers more effectively. Moreover, robotic surgery often results in shorter hospital stays and faster recovery times for patients, enabling them to return to their normal activities more quickly. Overall, the advantages of robotic surgery make it an increasingly popular choice for both surgeons and patients alike.
Endoscopic surgery is a minimally invasive procedure that is used to diagnose and treat various conditions of the urinary tract. There are several types of endoscopic surgery, including urethroscopy, cystoscopy, deflux injection into the bladder, ureteroscopy, percutaneous nephrolithotomy (PCNL), and lithotripsy.
Urethroscopy is a procedure that involves the insertion of a thin tube called an endoscope into the urethra. This allows the doctor to visually examine the urethra for any abnormalities or blockages. Urethroscopy can be used to diagnose and treat conditions such as urethral strictures or stones. Special precautions may need to be taken if the patient has a history of urinary tract infections or bleeding disorders.
Cystoscopy is a procedure that involves the insertion of a cystoscope, a thin tube with a camera and light, into the bladder through the urethra. This allows the doctor to visually examine the bladder for any abnormalities or conditions such as bladder stones or tumors. Cystoscopy can also be used to perform procedures such as bladder biopsies or the placement of stents. Special considerations may be necessary for patients with urinary tract infections or bladder obstructions.
Deflux injection into the bladder is a procedure that is used to treat vesicoureteral reflux (VUR), a condition where urine flows backward from the bladder into the ureters. During the procedure, a material called deflux is injected into the bladder to create a barrier and prevent urine from flowing backward. Special precautions may be necessary for patients with allergies to the materials used in the injection.
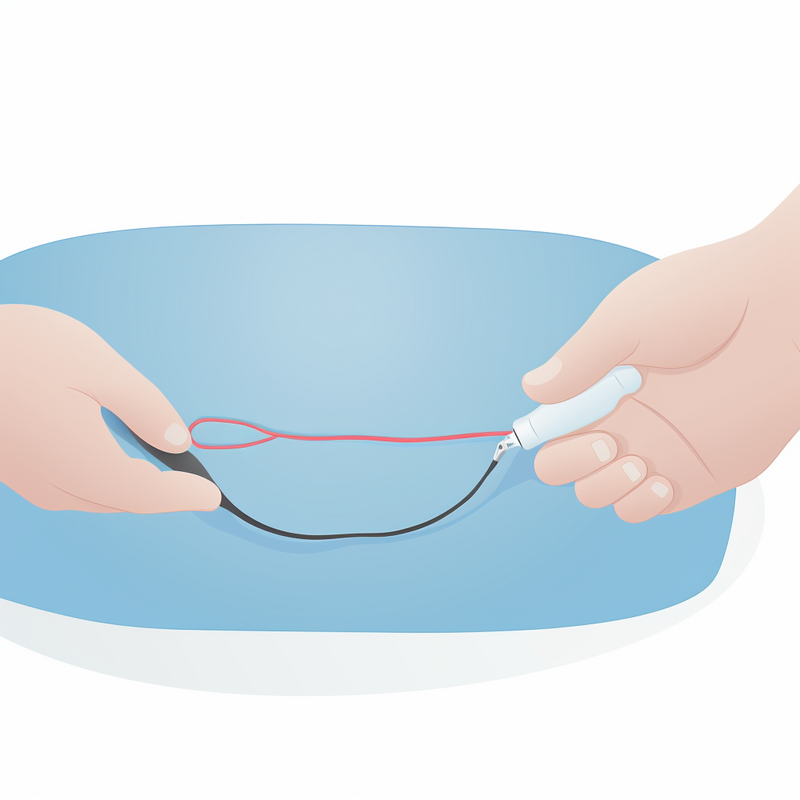
Ureteroscopy is a procedure that involves the insertion of a ureteroscope into the ureter, which is the tube that carries urine from the kidney to the bladder. This allows the doctor to visually examine the ureter for any abnormalities or conditions such as stones or tumors. Ureteroscopy can also be used to perform procedures such as stone removal or biopsies. Special considerations may be necessary for patients with kidney or urinary tract infections.
Percutaneous nephrolithotomy (PCNL) is a procedure that is used to remove large kidney stones. During the procedure, a small incision is made in the back and a tube is inserted into the kidney. This allows the doctor to remove the stone or break it up using tools such as lasers or ultrasound. PCNL is often used for stones that are too large to pass on their own or cannot be treated with other methods. Special precautions may be necessary for patients with bleeding disorders or kidney infections.
Lithotripsy is a procedure that is used to break up kidney stones using shock waves. During the procedure, the patient lies on a table and a machine directs shock waves at the kidney to break up the stones into smaller pieces. These smaller pieces can then pass through the urinary tract and be expelled from the body. Lithotripsy is often used for smaller stones that can be passed without surgery. Special considerations may be necessary for patients with bleeding disorders or kidney infections.
Overall, endoscopic surgery is a valuable tool for diagnosing and treating various conditions of the urinary tract. The specific type of endoscopic surgery chosen will depend on the individual's condition and the goals of treatment. Special considerations and precautions may need to be taken based on the patient's medical history and specific circumstances.
Endoscopic surgery in urology is a minimally invasive surgical procedure that utilizes tiny cameras and instruments inserted through natural body openings to diagnose and treat various urological conditions. This type of surgery focuses on managing kidney stones, as well as other conditions such as urinary tract infections, urethral strictures, and bladder tumors.
The use of endoscopic surgery allows urologists to visualize the urinary system without making large incisions. The cameras provide a clear view of the internal organs, aiding in the precise identification and removal of kidney stones or other abnormalities. Instruments such as lasers or robotic arms can be used to break the stones into smaller pieces for removal, reducing the need for traditional open surgery.
One of the significant advantages of endoscopic surgery is that it is particularly well-suited for treating pediatric patients. Children often suffer from urinary conditions such as kidney stones, and traditional open surgery can be traumatic for them. However, with the use of advanced technology and surgical instruments designed for children, endoscopic surgery offers a less invasive and more gentle approach to their healthcare.
In conclusion, endoscopic surgery in urology is a valuable technique that utilizes small cameras and instruments inserted through natural body openings to diagnose and treat various urological conditions. Its focus on managing kidney stones and other urological conditions, coupled with the advantages of using advanced technology and surgical instruments designed for children, make it an indispensable tool in urology.
Endoscopic surgery is a minimally invasive procedure used to treat various urological conditions. It involves the use of tiny cameras, scopes, and precise instruments to access and operate within the urinary system.
During the surgery, a small incision is made, and a thin, flexible tube called an endoscope is inserted. This endoscope contains a camera at one end, allowing surgeons to visualize the inside of the organ system. The camera transmits high-definition images to video screens, which display magnified images of the surgical field.
Simultaneously, the endoscope is equipped with adjustable scopes that can be manipulated to explore different angles and reach specific areas within the urinary system. This flexibility allows surgeons to navigate through narrow and complex structures with ease, enhancing surgical precision.
Precise instruments, such as tiny graspers, scissors, or laser probes, can be inserted through additional incisions to perform various surgical tasks. These instruments are specifically designed to enable delicate maneuvers inside the urinary system while minimizing trauma to surrounding tissues.
The use of video screens and magnified images greatly enhances the surgeon's ability to navigate through the organ system. It provides a clear and detailed view of the surgical site, enabling precise manipulation of instruments and precise incisions or sutures.
Overall, endoscopic surgery for urological conditions offers several benefits, including minimal scarring, reduced blood loss, shorter recovery time, and less postoperative pain. This procedure has revolutionized the field of urology, allowing for safer and more effective treatment of various urinary system disorders.
Introduction:
Minimally invasive surgery has revolutionized the field of urology, offering effective treatment options for various common urological conditions. This advanced surgical approach utilizes small incisions, specialized instruments, and advanced imaging technology to minimize tissue damage, reduce postoperative pain, and promote faster recovery. By exploring the following headings, we will gain an understanding of the common urological conditions that can be successfully treated using minimally invasive surgery techniques. From kidney stones to prostate enlargement, these procedures not only improve patients' quality of life but also provide an alternative to traditional open surgeries. With a focus on patient-centered care and optimal outcomes, minimally invasive surgery has become the preferred choice for urologists and patients alike.
Kidney stones, also known as renal calculi, are hard mineral and salt deposits that form in the kidneys. They can vary in size, from as small as a grain of sand to as large as a golf ball. Several factors contribute to the development of kidney stones.
Causes of kidney stones can include dehydration, certain medical conditions such as hyperparathyroidism or urinary tract infections, and certain medications or dietary habits. Symptoms of kidney stones can include severe pain in the back or side, blood in the urine, frequent urination, and cloudy or foul-smelling urine. Risk factors for kidney stones include a family history of the condition, a personal history of previous kidney stones, certain underlying medical conditions, and certain dietary factors such as a high sodium or high protein diet.
Two minimally invasive procedures commonly used to treat kidney stones are extracorporeal shock wave lithotripsy (ESWL) and ureteroscopic laser lithotripsy. ESWL involves using shock waves to break the kidney stones into smaller pieces that can be passed through urine. Ureteroscopic laser lithotripsy, on the other hand, utilizes a thin tube called a ureteroscope to directly visualize and break the kidney stones using laser energy.
The benefits of ESWL include its non-invasive nature, as it does not require any incisions, and its high success rates for kidney stones less than 2 centimeters in size. However, it may cause discomfort and pain during the procedure, and multiple sessions may be required to completely eliminate the stones.
Ureteroscopic laser lithotripsy offers the advantage of directly visualizing the stone and has a high success rate for stones larger than 2 centimeters. It also allows for the retrieval of any residual stone fragments. However, it requires general anesthesia, and there is a risk of complications such as ureteral injury or infection.
In conclusion, kidney stones are caused by a variety of factors, and their symptoms can be quite painful. ESWL and ureteroscopic laser lithotripsy are two minimally invasive procedures commonly used to treat kidney stones, each with their own set of benefits and limitations. It is important for individuals at risk for kidney stones to be aware of these treatment options and work closely with their healthcare providers to determine the most appropriate course of action.
Kidney stones, also known as renal calculi, are hard deposits made of minerals and salts that form in the kidneys. They can vary in size and shape and may be composed of different substances such as calcium, uric acid, struvite, or cystine.
Treatment options for kidney stones depend on various factors, including the size, location, and composition of the stone. One commonly used method is extracorporeal shock wave lithotripsy (ESWL), which uses sound waves to break the stones into smaller, more manageable pieces. This procedure is non-invasive and typically requires multiple sessions.
Another treatment option is ureteroscopic laser lithotripsy, which involves passing a thin tube called a ureteroscope through the urethra and bladder into the ureter or kidney. A laser fiber is then used to break up the stone into smaller fragments, which can be removed or passed naturally. This procedure is minimally invasive and allows for precise targeting of the stone.
Advancements in minimally invasive surgical techniques have revolutionized the treatment of kidney stones. These techniques, such as miniaturized instruments and robotic-assisted surgery, offer several benefits. They allow for smaller incisions, result in less tissue damage, reduce the risk of complications, and lead to shorter hospital stays and faster recovery times.
Each treatment option has its pros and cons. ESWL is non-invasive but may require multiple sessions and can cause discomfort. Ureteroscopic laser lithotripsy is minimally invasive but may not be suitable for larger stones or certain anatomical conditions.
A tailored approach to stone management is essential. Factors such as stone size, location, composition, patient preferences, and medical history should all be taken into account when determining the most appropriate treatment strategy. This may involve a combination of techniques, including dietary changes, medication, and surgical intervention, to optimize outcomes and minimize the risk of recurrence.
Overall, advancements in minimally invasive techniques have revolutionized the treatment of kidney stones, providing patients with effective options that offer shorter hospital stays, faster recovery times, and improved outcomes.